Every year, one of the leading causes of vision loss in the United States goes undetected and untreated among nearly 25% of older adults. Age-related macular degeneration (AMD) can rob people of their sight and, up until recently, has been detectable using only structural diagnostic eye tests. In the coming decades, the number of people with AMD is expected to more than double, impacting more than 22 million people in the U.S. alone.
The ability to diagnose and treat AMD at its earliest stages may help more patients preserve their quality of vision.
What Is Age-Related Macular Degeneration (AMD)?
As a chronic, progressive disease, age-related macular degeneration (AMD) is the leading cause of adult blindness in developed countries. It occurs when fatty deposits accumulate in the retina and block absorption of nutrients, such as vitamin A, necessary for normal cell function.
AMD affects the part of the retina responsible for central vision, called the macula. As the macula deteriorates, it becomes increasingly difficult to read, recognize faces, and see in dim light.
What Causes Age-Related Macular Degeneration?
Cholesterol deposits accumulate in the macula years before drusen are visible, making drusen the tip of the iceberg in AMD pathology.
Before drusen are visible, an invisible layer of cholesterol builds up between the pigmented layer of the retina (RPE) and the elastic layer of Bruch’s membrane. These cholesterol deposits — basal laminar (BLamD) and basal linear (BLinD) — cause oxidative stress and inflammation, hindering nutrient transportation to photoreceptor cells. As photoreceptor cells die, it becomes harder for the eyes to adjust to darkness, and night vision declines. This dark adaptation impairment is the first sign of AMD.
Prior to pivotal research conducted at the University of Alabama Birmingham, the Alabama Study on Age-Related Macular Degeneration (ALSTAR), AMD was staged as early, intermediate, and advanced. Thanks to the groundbreaking findings of this investigation, we can identify a subclinical stage of AMD.
Risk Factors for AMD
While no one knows exactly what causes age-related macular degeneration, there are a few factors that put older adults at risk for developing this condition.
- Age: Age is the greatest risk factor for AMD, especially for those over 50 years of age.
- Family history: Individuals with a family history of AMD are more prone to this disease. Several genes related to the development of AMD have been identified, showing that the disease has a hereditary component.
- Race: Caucasians have the greatest likelihood of developing AMD.
- Smoking: Smokers, ex-smokers and people regularly exposed to smoke are more likely to get AMD than those who never smoked.
- Obesity: Being overweight increases your risk of AMD, but those who are obese have a greater chance of progressing to the more severe form of the disease.
- Cardiovascular disease: Conditions that affect your heart and blood vessels may put you at a higher risk of AMD.
AMD Symptoms and Risk Factors
As the leading cause of adult blindness in developed countries, age-related macular degeneration is four times more prevalent than glaucoma and affects one in eight adults over age 60.ii Though common, it often goes undiagnosed until after significant, irreversible vision loss has occurred. Knowing the early symptoms of AMD is the first step toward proactive disease management to prevent the dramatic consequences of untreated disease.
AMD Symptoms
Some symptoms of macular degeneration are detected early, yet not connected to the disease until after the condition is fairly advanced. Other symptoms seem more obtrusive and are likely to trigger a visit to an eye care professional:
- Difficulty seeing at night
- Difficulty reading in dim light
- Worsened visual acuity
- Distorted vision
- Central vision loss
Dark Adaptation
Also known as “night blindness,” impaired dark adaptation is the earliest symptom of AMD. Physical changes that occur in the early development of AMD compromise the eye’s ability to adjust to darkness. This can make it difficult to drive at night, read in dim light, or adjust to dark places, like an unlit movie theater. More noticeable visual deficits become evident as the disease progresses, such as worsened visual acuity, distorted vision, and central vision loss.
AMD Risk Factors
There are also many risk factors associated with the development of AMD. Most risk factors can’t be modified, though others can be managed to some extent.
Non-modifiable Risk Factors:
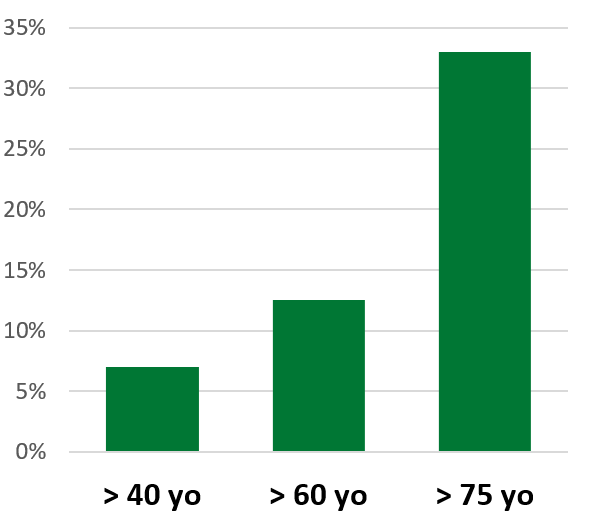
AMD Prevalence by Age ii
- Age 50 or older
- Family history of AMD
- Caucasian (white)
Age is the biggest risk factor for AMD. Family history, ethnicity, and gender can play a significant role as well. According to the National Eye Institute, AMD is more prevalent among white Americans as compared to other races. Perhaps partly due to life expectancy discrepancies, 65 percent of AMD cases in the U.S. were women in 2010.
Modifiable Risk Factors:
- Smoking
- High cholesterol
- Cardiovascular disease
- Diabetes
- Obesity
- Chronic sunlight exposure
The biggest modifiable risk factor for AMD is smoking. Current smokers carry a 2.5 to 4.8 times higher risk than non-smokers for developing AMD. Sadly, one study showed 90% of patients with AMD were not advised to stop smoking and less than 50% of smokers know smoking may contribute to blindness.
Based on epidemiological studies, several systemic conditions carry an increased risk of developing AMD. Keeping cardiovascular disease, diabetes, high cholesterol, and obesity in check may help preserve the vision in these patients, as well as improve their quality of life.
Advancements in AMD Testing
Over the past several decades, the eye care industry made tremendous advances in the ability to test for and diagnose age-related macular degeneration (AMD).
Types of AMD Tests
While not exhaustive, below is an overview of current methods used to assess, diagnose and monitor AMD.
Functional Assessment
Functional testing for impaired dark adaptation not only helps to accurately det
ect AMD at a subclinical stage, it is also a tool used to monitor the disease and measure treatment effectiveness.
- Dark Adaptation
Structural Evaluations
Several imaging tests are used to evaluate physical changes in the macula. These can detect and monitor drusen formation and changes in size, plus geographic atrophy (GA) and neovascularization in later stages.
- Clinical Examination with Slit Lamp
- Fundus Fluorescein Angiography (FFA)
- Optical Coherence Tomography (OCT)
- Fundus Autofluorescence Imaging (AF)
Risk Factor Testing
Several tests can be administered to assess the likelihood of developing AMD. These are not diagnostic tools, but are used to identify patients with higher risk for macular degeneration.
- Macular Pigment Optical Density (MPOD)
- Family History
- Genetic Testing
Late-Stage Progression Tools
Though useful for monitoring progression in the late stages of the disease, these tests are not considered sensitive enough to diagnose AMD at an early stage.
- Visual Acuity
- Amsler Grid
- Contrast Sensitivity
- ERG
- Macular Visual Field
- Microperimetry
- Color Vision
Testing for Subclinical AMD
Diagnosing the earliest stages of AMD can present a challenge because patients are often asymptomatic, have good corrected visual acuity and the retina looks normal upon structural evaluation. Consequently, a routine vision test and structural evaluations may not raise any suspicion of the disease.
Fortunately, we now know that impaired dark adaptation function is the earliest biomarker of AMD—with impairment taking place at a subclinical level at least three years before drusen are visible. By measuring dark adaptation function in patients over age 50—especially when presenting with night vision complaints—eye care professionals can now detect subclinical AMD before any damage has been done. Once subclinical AMD is diagnosed, disease progression can be slowed through early treatment and proactive disease management.
Early Detection with AdaptDx Pro
AdaptDx Pro™ is the only test for dark adaptation that can be used quickly and effectively in a clinical setting. It uses an objective functional measure called the Rod Intercept™ (RI). Unlike traditional dark adaptation testing, the AdaptDx Pro Rapid Test takes less than 6.5 minutes. Easy to administer and interpret, it is reimbursable and detects AMD with 90.6% accuracy.
Using a single number, the Rod Intercept, you can identify dark adaptation consistent with AMD before your patient experiences irreversible vision loss.
